Core Evidence & Research
Core Evidence & Research
There is a wealth of evidence supporting the effectiveness of DBT. The first randomized controlled trial (RCT) of DBT was published in 1991, in which Dr. Marsha Linehan and her colleagues found that DBT resulted in significant improvements for chronically suicidal and self-injuring women with borderline personality disorder, a clinical population that had previously been viewed as untreatable (Linehan et al., 1991).
In the decades since this landmark study, DBT has been extensively researched for individuals with a wide range of mental health conditions receiving treatment in diverse practice settings around the world.
Understanding Research Related to DBT
There are multiple research domains for DBT studies, including:
- Efficacy Trials: Efficacy research is aimed at understanding whether an intervention produces the expected result under ideal circumstances. Control over those circumstances protects the internal validity of the study. Most efficacy trials of DBT were completed in academic research settings. The efficacy trials listed below are randomized controlled trials (RCTs). For a summary that includes other types of efficacy studies (e.g., quasi-experimental studies), please refer to the Non-RCT Research Data.
- Effectiveness Trials: Effectiveness research is aimed at measuring the degree of “beneficial effect” in a real-world setting. These studies focus on external validity or how well the results can be expected to generalize to different settings. Effectiveness trials of DBT are most often completed in community practice settings. The list below only includes randomized controlled trials (RCTs). For a summary that includes other types of effectiveness studies (e.g., quasi-experimental studies), please refer to Non-RCT Research Data.
- Dissemination & Implementation: Dissemination research is the systematic study of how to distribute information and intervention materials to a specific audience to increase knowledge and use of evidence-based interventions. Implementation research is the systematic study of methods of promoting the adoption and integration of evidence-based interventions into routine clinical practice settings. This type of research uses multiple disciplines and methods. Implementation research focuses on practical approaches to increase the use of evidence-based interventions and enhance equity, efficiency, and sustainability.
- Mechanisms of Action: Research evaluating mechanisms of action aims to identify the variables or processes through which a treatment produces a change in desired outcomes. Research evaluating predictors of outcome aims to identify variables that are associated with better or worse treatment outcomes.
- Meta-Analyses & Systematic Reviews: Systematic reviews provide a comprehensive review of the literature based on systematic searches of relevant research databases. Meta-analyses combine data from multiple studies to evaluate treatment effects across studies.
- Differing Levels of Rigor & Credibility: Ensuring that DBT is delivered adherently is an important aspect of quality assurance. In particular, it enables administrators, programs, therapists, and consumers to know that the treatment being delivered is actually DBT. In addition, therapist adherence to DBT has been shown to improve client outcomes, including reducing suicide attempts, psychiatric hospitalizations, substance use, and treatment dropout [6-8]. Therefore, delivering DBT with adherence is a critical component of providing high quality DBT and achieving the best possible outcomes for clients.
Click here for our list of References for DBT Foundational and Intensive Training.
Randomized Control Trials Since 2013
Research Archives
Archived DBT Research from Behavioral Tech Institute:
RCT and Non-RCT Summaries
Due to popular demand, we are making this archive of printable summaries of RCT and non-RCT studies available, however please note that it was last updated in 2016. In treatment research, a randomized controlled trial is a study in which patients or clients are randomized to one of two groups: the intervention being evaluated and an alternative treatment.
- RCT Research Data: Standard DBT (4 Modes of Treatment)
• This list is current as of 2016. - RCT Research Data: Skills-Only DBT
• This list is current as of 2016. - Non-RCT Research Data
•This list is current as of 2013.
A Skills Deficit Model
DBT assumes that many of the problems exhibited by clients are caused by skills deficits. In particular, the failure to use effective behavior when it is needed is often a result of not knowing skillful behavior or when or how to use it. For example, deficits in emotion regulation skills are believed to be a core problem in individuals with borderline personality disorder, and these deficits result in the use of maladaptive behaviors to regulate emotions (e.g., suicide attempts, non-suicidal self-injury, substance use). Therefore, a key focus in DBT is to improve clients’ ability to use skillful behavior when needed, with a particular focus on learning effective emotion regulation strategies.
Full-model DBT is still the standard of treatment for highly suicidal clients, as it has the preponderance of evidence. Even clients in skills-only studies generally received intensive case management that served some of the functions of individual therapy.
However, consistent with this skills deficit model, use of DBT skills has been found to fully or partially explain improvements during standard DBT and DBT skills training in problems such as suicidal behavior, non-suicidal self-injury, depression, anger control, emotion dysregulation, and anxiety (Neacsiu et al., 2010; Neacsiu et al., 2014). In addition, improvements in emotion regulation (Axelrod et al., 2011), experiential avoidance (Berking et al., 2009), and assertive anger (Kramer et al., 2015) have been found to account for changes in outcomes such as substance use, depression, and social functioning during DBT. Taken together, these findings suggest that DBT works because it successfully increases clients’ ability to use effective coping skills, particularly strategies for expressing, experiencing, and regulating intense emotions.
DBT as an Effective Treatment
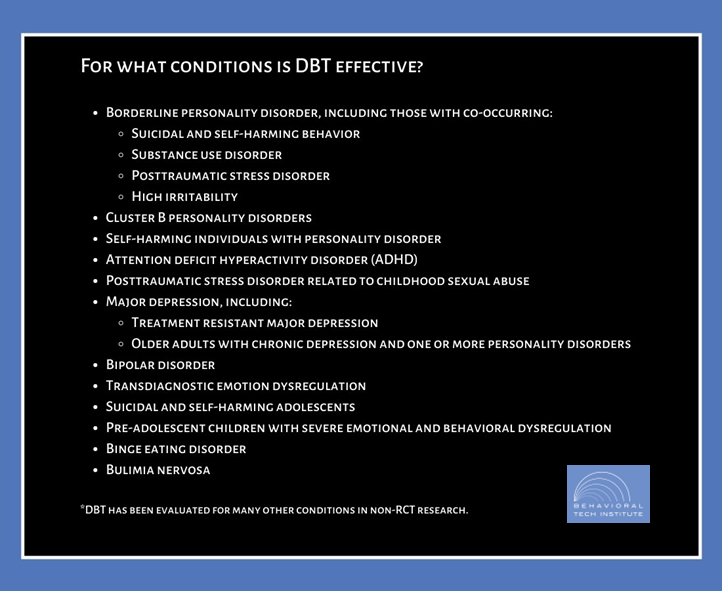
Although the strongest evidence exists for DBT as a treatment for people with borderline personality disorder, DBT has been found to be effective for a wide variety of mental health conditions. Conditions for which standard or adapted versions of DBT have been found to be effective in at least one randomized controlled trial are listed below.
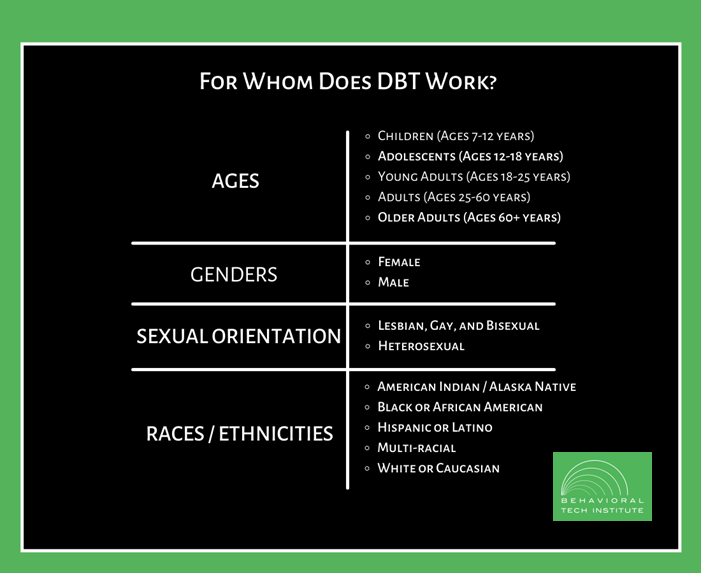
DBT has been evaluated and found to be effective among individuals from diverse backgrounds in terms of age, gender, sexual orientation, and race/ethnicity. The demographic groups listed below have made up a sizeable proportion (25-100%) of the sample in at least one study of DBT.
Although DBT was originally developed and researched in the United States, it has since been evaluated in many randomized controlled trials (RCTs) conducted in other regions and countries, including:

AUSTRALIA
• BPD & NSSI
• Ages: 18-65

CANADA
• BPD & NSSI/SA
• Bipolar I or II
• ED & SUD
• Ages: 18-60
DENMARK
• BPD Traits & recent SA

GERMANY
• PTSD; BPD Traits
• Ages: 17-65

THE NETHERLANDS
• BPD
• SUD
• Ages: 18-70
NORWAY
• BPD Traits & NSSI/SA
• Ages: 12-18
SPAIN
• BPD
• Ages 18-45

SWEDEN
• ADHD
• Ages: 18 or older
TAIWAN
• Depression, BPD & SA
• College students
UNITED KINGDOM
• Cluster B PD
• PD & NSSI
• Ages: 16-65
UNITED STATES
• BPD, NSSI, SA, SUD, Depression, Bipolar, PTSD, Binge eating & BN, ADHD; Abuse; DMDD
• Ages 7-80
AUSTRALIA
- BPD & NSSI
- Ages: 18-65
CANADA
- BPD & NSSI/SA
- Bipolar I or II
- ED & SUD
- Ages: 18-60
DENMARK
- BPD Traits & recent SA
GERMANY
- PTSD; BPD Traits
- Ages: 17-65
THE NETHERLANDS
- BPD
- SUD
- Ages: 18-70
NORWAY
- BPD Traits & NSSI/SA
- Ages: 12-18
SPAIN
- BPD
- Ages 18-45
SWEDEN
- ADHD
- Ages: 18 or older
TAIWAN
- Depression, BPD & SA
- College students
UNITED KINGDOM
- Cluster B PD
- PD & NSSI
- Ages: 16-65
UNITED STATES
- BPD, NSSI, SA, SUD, Depression, Bipolar, PTSD, Binge eating & BN, ADHD; Abuse; DMDD
- Ages 7-80
These international RCTs have found that DBT is effective when implemented in other cultures and results are similar to those found in studies conducted in the United States. For example, DBT has been found to be superior to treatment as usual in Great Britian, the Netherlands, Australia, and Norway.
Resources
Assessment Instruments Used in DBT Research
In order to increase the ability to make comparisons across studies, it is important that DBT researchers use the same assessment instruments. The links below include information about assessment instruments most commonly used in DBT research.
- Annotated Bibliography of Assessment Instruments
- Assessment Instruments from the BRTC at the University of Washington
Annual Research Conferences
DBT research is presented at many conferences around the world each year. Some of the most common conferences attended by DBT researchers are:
- International Society for the Improvement and Teaching of DBT (ISITDBT)
- Association for Behavioral and Cognitive Therapies (ABCT)
- International Congress on Borderline Personality Disorder and Allied Disorders (from ESSPD)
- American Association of Suicidology (AAS)
- Society for Implementation Research Collaboration (SIRC)
- North American Society for the Study of Personality Disorders (NASSPD)
- International Society for the Study of Personality Disorders (ISSPD)
- International Society for the Study of Self-Injury (ISSS)
Research Journals
DBT research has been published in a wide range of journals that span multiple disciplines. The journals listed below either specialize in topics directly relevant to DBT or have published prominent DBT research.
- JAMA Psychiatry
- Journal of Consulting and Clinical Psychology
- Behaviour Research and Therapy
- Behavior Therapy
- American Journal of Psychiatry
- Borderline Personality Disorder and Emotion
- Journal of Personality Disorders from ISSPD
Suicide Data and Statistics
Data on suicide and self-inflicted injury are an important tool in intervention and prevention efforts. Find the latest information from:
- U.S. Centers for Disease Control and Prevention: Suicide and self-inflicted injury
- National Institute of Mental Health: Statistics
